- @NGRI Metro Stn, Piller No: C-964, St No: 7,
Habsiguda, Hyderabad - 500 007, TS INDIA.
Bhargavi PRO (Telugu, English, Hindi)
+91-76610 86644Admin / PRO (Telugu, English, Hindi)
+91-76610 17755Pro's IUI/IVF/ICSI (Telugu, English)
+91-76610 58800Divakar Reddy (CEO) (Telugu, English, Hindi)
+91-98483 43244SINDHU (PRO) (English, Telugu, Hindi)
+91-79819 36828Get An Appointment
ICSI
Patrons Please Note:
Bhargavi PRO (Telugu, English, Hindi)
+91-76610 86644Admin / PRO (Telugu, English, Hindi)
+91-76610 17755Pro's IUI/IVF/ICSI (Telugu, English)
+91-76610 58800Divakar Reddy (CEO) (Telugu, English, Hindi)
+91-98483 43244Enquiry
| Total Cases Done | Successful | Success Rate |
|---|---|---|
0
|
0
|
0%
|
First Attempt Successful
| Total Cases Successful | First Attempts | First Attempt Success % |
|---|---|---|
0
|
0
|
0%
|
ICSI (Intracytoplasmic Sperm Injection)
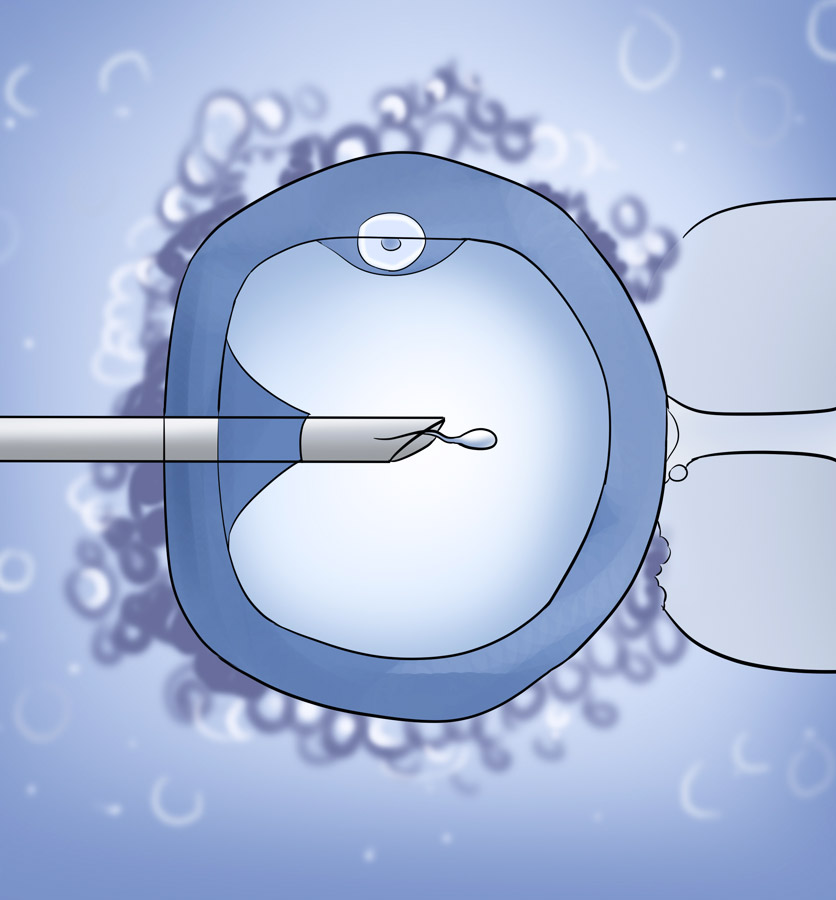
With very low sperm count in the 1990s, (less than 5 million per ml) or having poor quality sperm, fathering children was a difficult process at this time. This concerning issue got a breakthrough with ICSI, which took place in Brussels, Belgium in 1992.
Ever since, many couples have been able to become fathers of their own children. In Intracytoplasmic Sperm Injection (ICSI) steps are mostly similar to In Vitro Fertilization (IVF), except the process of fertilization.
Most often, in In Vitro Fertilization (IVF) one egg is combined with 100,000 sperms and one of the sperms takes the process of fertilization with the egg on its own.
On the contrary, in the process of ICSI, each egg is held and injected with a single live sperm. This micro-fertilization is performed with the aid of a machine called the Micromanipulator.
ICSI is done where the egg is held and injected with a single live sperm, cultured for 2-3 days and premium quality of embryos are transferred in the uterus.
- 1. Severely low sperm counts
- 2. Poor quality of sperms
- 3. Failed Fertilization in IVF
- 4. Males with azoospermia
Where there is no sperm present in the semen, or the azoospermia may be of obstructive type, in which there is production of sperms in the testis, but blockage of the conduction system. This brings the sperm out into the semen.
Alternatively, the azoospermia may be of the non-obstructive type. In this type, there is a failure of the testis to produce sperms. In these days, it is found that in both these types of azoospermia, sperms can be isolated directly from the testis, with the aid of using the sperm retrieval Techniques of PESA/TESA /TESE.
At Dr. Padmaja Fertility (IVF) Centre, we believe in performing ICSI on patients who have had a previous history of tuberculosis or endometriosis.
It gives better fertilization rates than standard In Vitro Fertilization (IVF).
In modern days, some units are advocating routine ICSI for all patients, even among those who are doing good with normal sperm counts.
We refrain from such practice as we opine that pregnancy is required to be achieved with minimum handling of the gametes outside the body.
If the sperm count, if it is in the grey-one area, we may have to subject half the eggs to In Vitro Fertilization IVF and half the eggs to ICSI.
We find that our success rates are in the range of 35 to 40% among azoospermia and non-azoospermia patients, which are comparable to the best in the world.